
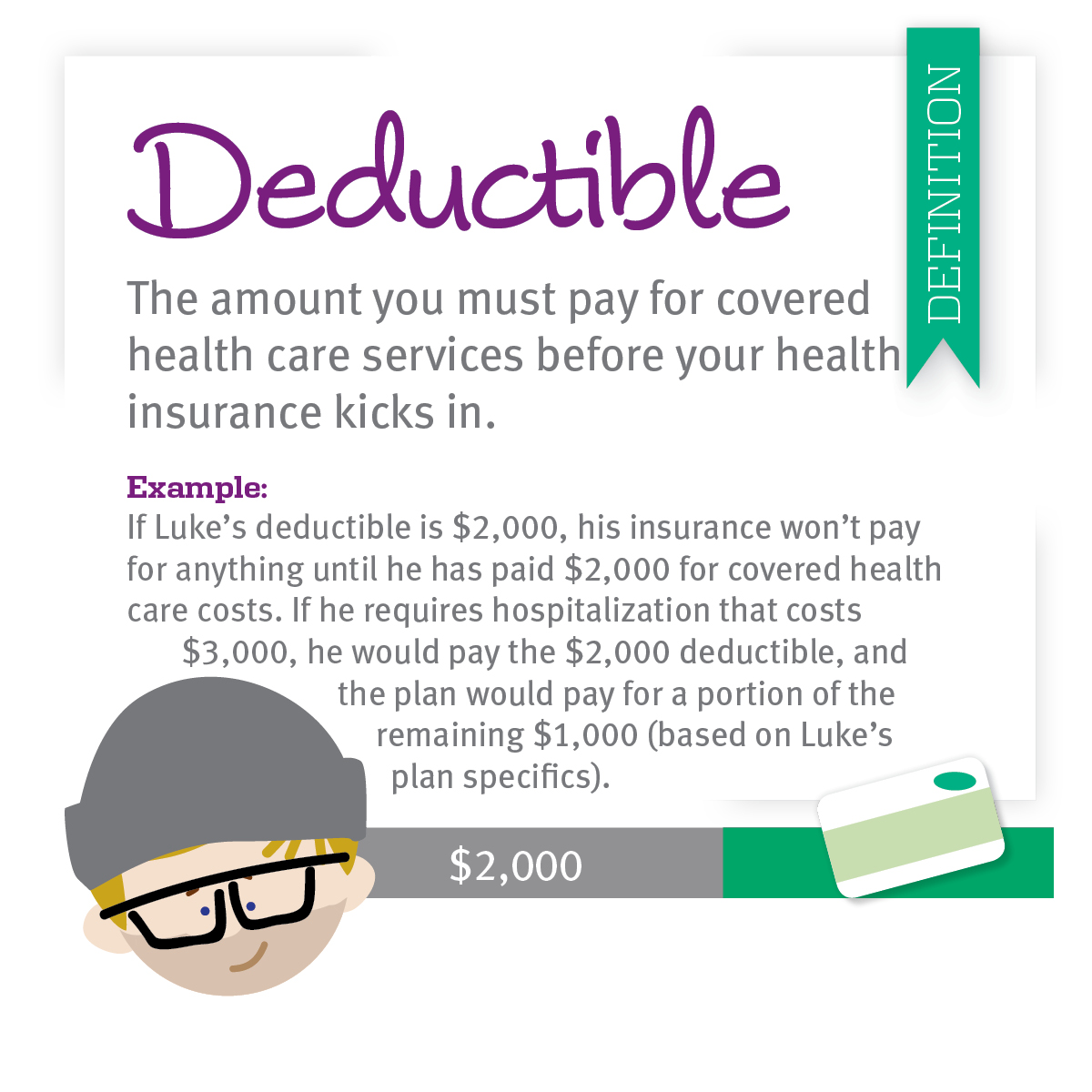
The term precertification here means the utilization review process to determine whether the requested service, procedure, prescription drug or medical device meets the company's clinical criteria for coverage.Should the following terms and conditions be acceptable to you, please indicate your agreement and acceptance by selecting the button below labeled "I Accept". In the event that a member disagrees with a coverage determination, member may be eligible for the right to an internal appeal and/or an independent external appeal in accordance with applicable federal or state law. Medical necessity determinations in connection with coverage decisions are made on a case-by-case basis. Please note also that the ABA Medical Necessity Guide may be updated and are, therefore, subject to change. Some plans exclude coverage for services or supplies that Aetna considers medically necessary. The member's benefit plan determines coverage. The conclusion that a particular service or supply is medically necessary does not constitute a representation or warranty that this service or supply is covered (i.e., will be paid for by Aetna) for a particular member. Members and their providers will need to consult the member's benefit plan to determine if there are any exclusions or other benefit limitations applicable to this service or supply. Members should discuss any matters related to their coverage or condition with their treating provider.Įach benefit plan defines which services are covered, which are excluded, and which are subject to dollar caps or other limits. Treating providers are solely responsible for medical advice and treatment of members. The ABA Medical Necessity Guide does not constitute medical advice. The Applied Behavior Analysis (ABA) Medical Necessity Guide helps determine appropriate (medically necessary) levels and types of care for patients in need of evaluation and treatment for behavioral health conditions. However, these plans usually charge copays for things like doctor visits, prescriptions, emergency room visits, and hospitalizations.By clicking on “I Accept”, I acknowledge and accept that: Some health plans, particularly some employer-sponsored health maintenance organizations (HMOs), don't require a deductible at all. STI prevention counseling for adults who are at high risk.Screenings for certain sexually transmitted infections (STI), such as chlamydia, gonorrhea, hepatitis B, and syphilis depending on age, sex, and risk.Alcohol misuse screening and counseling.Cholesterol screening for those considered high risk or of certain ages.Type 2 diabetes screenings for those ages 40 to 70 who are overweight or obese.Routine immunizations as recommended by age.Colorectal cancer screenings, such as a colonoscopy once you turn 45.
#HEALTH INSURANCE COPAY AFTER DEDUCTIBLE PROFESSIONAL#
Breast cancer mammogram screenings every two years for females 50 and over, and as recommended by a healthcare professional for females age 40 to 49 or those at higher risk for breast cancer.Some of the covered preventive care under the ACA includes:


 0 kommentar(er)
0 kommentar(er)
